Dementia is incorrectly believed to be an inevitable part of the biological aging process and a condition that occurs only in the elderly. But a recent UK study highlights different risk factors by age—and that adults in their 50s should be aware that diabetes (and resulting high blood pressure) can increase the risk of developing the brain disorder.
While diabetes can occur at any age, weight gain and inactivity affect people in their 50s in greater numbers—and each increases the risk of cardiovascular disease, heart attack and stroke.
Not only can diabetes raise the risk of heart disease and stroke (which can lead to damaged blood vessels in the brain), but too much insulin can affect brain chemical balance. High blood sugar can also cause inflammation that can damage brain cells.
A 30-year survey conducted by Seattle-based Adult Changes in Thought (ACT) also implicated diabetes in dementia onset. The researchers identified and quantified multiple factors affecting brain aging that included hearing and vision loss, hypertension, alcohol consumption, obesity, depression and social isolation, physical inactivity, blood sugar levels and diabetes.
They found that higher glucose levels led to an 18% increased risk of Alzheimer’s and dementia in adults without diabetes and a 40% increased risk for those with diabetes. The diabetes and dementia correlation is clear: Prevention should be the goal, so paying attention to symptom onset is key.
The diabetes and dementia correlation is clear: Prevention should be the goal, so paying attention to symptom onset is key.
Prediabetes is a warning sign
Long before a diabetes diagnosis, people first develop prediabetes—a condition where blood sugar levels are higher than normal, but not high enough to be diagnosed as type 2 diabetes. This is the window in which making lifestyle changes is the best method to avoid developing full-blown type 2 diabetes.
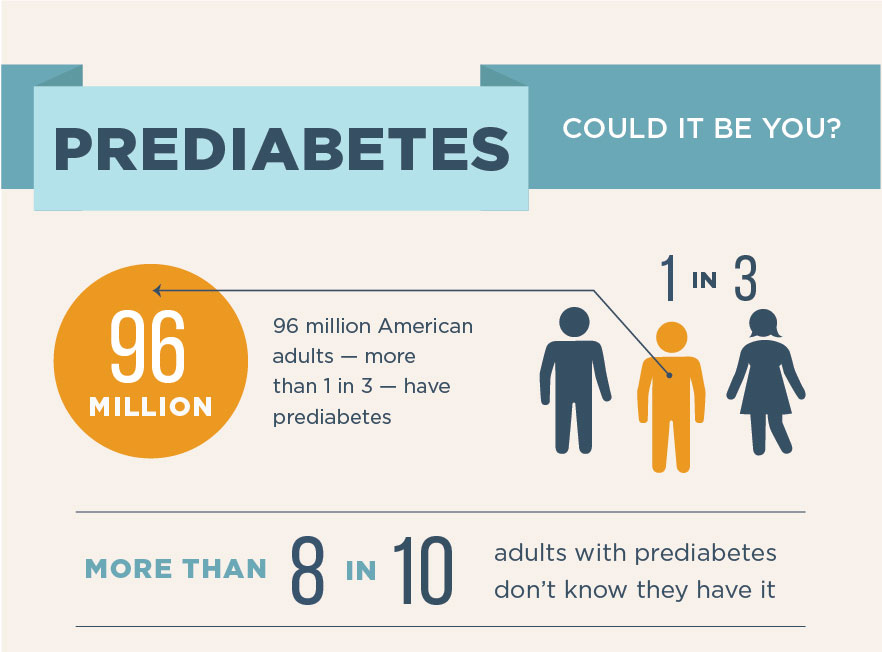
Approximately 96 million American adults – more than one in three – have prediabetes, and 80% are unaware they may have developed the condition.
Approximately 96 million American adults – more than one in three – have prediabetes, and 80% are unaware they may have developed the condition.
But what causes prediabetes? Insulin is a hormone made by your pancreas that acts like a key to let blood sugar into cells for use as energy. If you have prediabetes, however, your body’s cells don’t respond normally to insulin. The pancreas then increases insulin production to get cells to respond. Eventually, the pancreas can’t keep up, and your blood sugar rises, setting the stage for prediabetes and type 2 diabetes.
You can have prediabetes for years with no symptoms; it’s often undetected until serious health problems like type 2 diabetes are diagnosed. It’s important to speak to your doctor about scheduling blood sugar tests if you have any of the risk factors for prediabetes.
Prediabetes risk factors:
- Being overweight and exceeding optimal BMI
- Being 45 years or older
- Having a parent, brother or sister with type 2 diabetes
- Being physically active less than three times a week
- Ever having gestational diabetes (diabetes during pregnancy) or giving birth to a baby weighing more than nine pounds
- Having polycystic ovary syndrome
Race and ethnicity are also a factor, as African Americans, Hispanic/Latino Americans, American Indians, Pacific Islanders, and some Asian Americans are at higher risk.
Common symptoms of type 2 diabetes
Think you might have type 2 diabetes? The most common symptoms typically include:
- Unusual thirst or hunger
- Frequent urination
- Fatigue
- Blurry vision
- Weight loss
Your doctor may order multiple tests to determine blood sugar levels as recommended by the CDC, including:
A1C test
The A1C test measures average blood sugar levels over the past two or three months. An A1C below 5.7% is normal, between 5.7 and 6.4% indicates you have prediabetes, and 6.5% or higher indicates you have diabetes.
Fasting blood sugar test
This measures blood sugar after an overnight fast (not eating). A fasting blood sugar level of 99 mg/dL or lower is normal, 100 to 125 mg/dL indicates you have prediabetes, and 126 mg/dL or higher indicates you have diabetes.
Glucose screening test
This measures blood sugar at the time of the test. After drinking a liquid that contains glucose, your blood will be drawn an hour later to check blood sugar levels. A normal result is 140 mg/dL or lower. If your level is higher than 140 mg/dL, you’ll need to take a glucose tolerance test.
Glucose tolerance test
This measures blood sugar before and after you drink a liquid that contains glucose. You’ll fast (not eat) overnight before the test and have blood drawn to determine the fasting blood sugar level. Then you’ll drink the liquid and have blood sugar levels checked one hour, two hours and possibly three hours after. At two hours, a blood sugar level of 140 mg/dL or lower is considered normal, 140 to 199 mg/dL indicates you have prediabetes, and 200 mg/dL or higher indicates you have diabetes.
Random blood sugar test
This measures blood sugar at the time you’re tested. You can take this test at any time and don’t need to fast first. A blood sugar level of 200 mg/dL or higher indicates you have diabetes.
Action steps to prevent prediabetes and type 2 diabetes
Medical experts and health coaches all agree the following steps are essential for diabetes prevention:
Get active – Recommended exercise for an adult in their 50s is a minimum of 150 to 300 minutes per week.
Eat better – A healthy diet is one of the best weapons for fighting weight gain. Diets recommended for both cardiac disease and diabetes include low-glycemic, high-fiber foods and filled with colorful fruits and vegetables, healthy fats and lean proteins. The MIND diet is focused on food groups that protect the brain from age-related problems like Alzheimer’s disease.
Lose weight – Your physician can help calculate optimal BMI and weight. When you shed fat and unnecessary pounds, the burden on the heart, lungs, blood vessels and skeleton are reduced.
While the risk of dementia increases as we age, medical experts say that age 50 is a good time to address disease prevention and chronic health problems to take preventive steps now. Losing pounds and maintaining an optimal weight, adopting good nutrition and sleep hygiene habits, and choosing a health-supportive lifestyle will mitigate chances of developing both diabetes and cardiac disease and lessen risks of developing dementia.
Diabetes Glossary
Learn more about diabetes and common terms associated with the condition at www.webmd.com/diabetes/diabetes-glossary-terms.